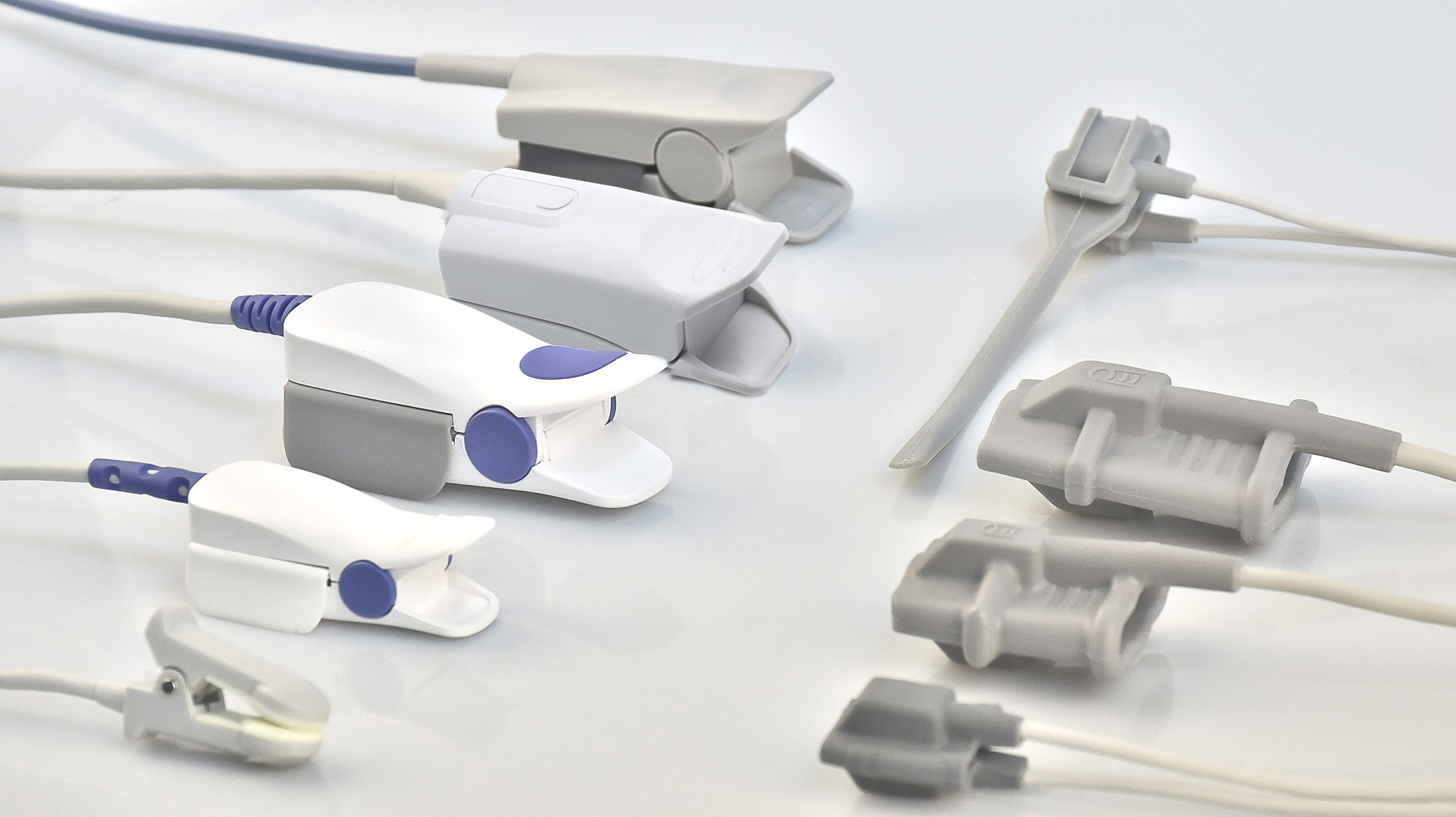
Key Features of Clinical-Grade SpO2 Sensors
Accuracy Standards for Oxygen Saturation Measurement
Clinical-grade SpO2 sensors are crucial for precise oxygen saturation measurement and must abide by rigorous accuracy standards established by bodies like ISO and CE. These standards typically require the device to maintain an accuracy within ±2% of the true blood oxygen saturation level. To achieve this, regular calibration and adherence to regulatory guidelines are essential, ensuring the accuracy and reliability of these sensors over time. With proper maintenance, these devices play a pivotal role in clinical settings, impacting patient care and outcomes significantly.
Signal-to-Noise Ratio Optimization in SpO2 Probes
The signal-to-noise ratio (SNR) in SpO2 probes is a key factor in achieving reliable oxygen saturation readings, especially in patients with low perfusion. A high SNR ensures that the desired signal is strong in comparison to background noise, which is vital for accurate measurements. Several techniques, such as digital filtering and advanced algorithm implementations, are employed to enhance the SNR in clinical environments. These optimizations ensure that readings remain precise and dependable, regardless of external interferences, which is particularly important in sensitive medical settings.
Clinical Validation Requirements for Medical Use
Clinical validation is an integral process for verifying the reliability and accuracy of SpO2 sensors intended for medical use. This process involves extensive testing across diverse patient populations to ensure the broad applicability and effectiveness of the sensors. Documenting these validation studies is crucial as it forms the basis for obtaining regulatory approval and facilitates the clinical adoption process. By demonstrating a sensor’s reliability through rigorous testing, manufacturers can assure healthcare providers of its performance, ultimately aiding in better patient management and care.
Factors Influencing Sensor Performance
Impact of Skin Pigmentation on Light Absorption
Skin pigmentation can significantly influence the performance of SpO2 sensors due to its role in light absorption. In fact, variations in skin color can lead to discrepancies in oxygen saturation readings. Recent studies published in medical journals suggest that individuals with darker skin tones may experience less accurate measurements. This inaccuracy arises because melanin, the pigment responsible for skin color, absorbs more light, thereby affecting the sensor's readings. To address these disparities, adjustments in sensor design and algorithmic calibration are crucial, ensuring that SpO2 devices provide accurate results across all skin tones.
Effects of Nail Polish & Artificial Nails
Nail polish and artificial nails can interfere with SpO2 readings by obstructing light transmission, which is essential for accurate measurement. Tests have shown that particularly dark-colored nail polish can significantly mislead the sensor readings. This interference occurs because the polish can alter the way light passes through the nail, skewing the detection of blood oxygen levels. Therefore, it is recommended to remove nail polish prior to testing to ensure accurate results. Additionally, artificial nails may have a similar effect, thereby necessitating removal for precise SpO2 measurement.
Peripheral Circulation Challenges
Conditions affecting peripheral circulation, such as hypothermia and shock, can lead to poor SpO2 readings. These conditions result in reduced blood flow to extremities like fingers and toes, where SpO2 sensors are typically applied. This lack of adequate blood flow can lead to unreliable or falsely low oxygen saturation levels. Understanding these challenges is critical for healthcare providers, enabling them to make informed interpretations of SpO2 readings. In cases where circulation is compromised, alternative methods of oxygen saturation measurement or sensor adjustments may be necessary to obtain accurate readings.
Temperature Probe Integration Considerations
Integrating temperature probes with SpO2 sensors enhances patient monitoring capabilities by providing a comprehensive assessment of a patient's respiratory and metabolic state. This combination allows healthcare providers to monitor vital signs simultaneously, offering a well-rounded view of patient health. However, technical considerations must be made to ensure the accuracy of both measurements, especially in real-time applications. Proper integration involves synchronizing data from both sensors, ensuring each provides precise readings without interference, ultimately leading to more effective patient management.
Addressing Racial Disparities in Pulse Oximetry
Clinical Studies on Melanin Interference
Recent clinical studies have illuminated the effects of melanin on pulse oximetry readings, especially in individuals with darker skin. These studies suggest that the melanin present in darker skin tones can absorb more of the red and infrared light emitted by pulse oximeters, leading to potentially inaccurate readings. For instance, a study at the University of Michigan has shown that Black patients were nearly three times more likely to have hidden hypoxemia than their White counterparts. This emphasizes the need for recalibrating these devices to cater to a diverse demographic, ensuring that the measurements are consistently accurate across all skin tones. Continuous research is vital in this area to develop more inclusive health technologies that accurately reflect the health parameters of diverse racial groups.
NIH Recommendations for Diverse Testing Populations
The National Institutes of Health (NIH) has set forth recommendations to emphasize the importance of including diverse populations in the testing of pulse oximetry devices. These guidelines are designed to ensure that pulse oximeters provide reliable readings across various ethnicities, thus reducing healthcare disparities. Implementing such recommendations involves rigorous testing of these devices to reflect true performance in real-world conditions where patients' skin tones vary. In doing so, the healthcare industry can move towards more equitable diagnostics, reducing the gap in racial disparities. By adhering to NIH standards, manufacturers can enhance the accuracy of medical readings and contribute to improved health outcomes for all populations.
FDA Guidelines for Medical Oxygen Sensors
Prescription vs. Over-the-Counter Device Standards
The FDA differentiates regulatory standards for prescription devices and over-the-counter SpO2 sensors. Prescription devices often undergo more rigorous testing processes to ensure safety and efficacy before reaching healthcare professionals and patients. In contrast, over-the-counter devices face less stringent regulations, which can impact their reliability. Healthcare professionals must understand these distinctions to select the appropriate device for patient care, ensuring that oxygen sensors meet individual needs and maintain high standards of clinical reliability.
Blood Gas Test Correlation Requirements
SpO2 sensors are required to correlate with arterial blood gas test results for clinical reliability. The FDA mandates validation studies that compare pulse oximetry readings to blood gas measurements, ensuring that they are accurate and trustworthy. Such correlations are crucial for making clinical decisions regarding patient care based on SpO2 readings. By adhering to these requirements, healthcare providers can enhance patient safety and improve treatment outcomes.
Upcoming Regulatory Changes for SpO2 Probes
The FDA is in the process of updating regulations for SpO2 probes, aiming to enhance patient safety and device accuracy. Understanding and adapting to these regulatory changes is vital for manufacturers and clinics to maintain compliance and improve healthcare outcomes. Emerging regulations are expected to focus on improving accuracy standards and enhancing usability, thereby offering more reliable medical devices across the healthcare sector.
Best Practices for Clinical Implementation
Proper Sensor Placement Techniques
Correct placement of SpO2 sensors is crucial for obtaining accurate readings in clinical settings. Sensor positioning directly affects the reliability of oxygen saturation measurements, making it essential for healthcare professionals to be adept in optimal application techniques. Training programs should emphasize the importance of proper alignment and contact with the skin to avoid misleading results and unnecessary clinical interventions. Misalignment can cause false alarms or inaccurate readings, potentially leading to inappropriate medical decisions.
Calibration Protocols with EEG Electrodes
Calibrating SpO2 sensors alongside EEG electrodes enhances the accuracy of multi-modal monitoring. By synchronizing the readings of these devices, healthcare providers can gain a comprehensive view of a patient's health status. Establishing standardized calibration protocols ensures that all devices deliver reliable and consistent performance, crucial in critical care environments. Such protocols are essential for maintaining the integrity of data collected from multiple monitoring devices, thus aiding in precise clinical assessments.
Multi-Parameter Monitoring Synergy
Implementing synergy between SpO2 sensors and other monitoring devices significantly enhances patient care by providing a multi-faceted view of patient health. Multi-parameter monitoring facilitates timely interventions and comprehensive assessments, as it allows clinicians to observe various physiological parameters simultaneously. The successful integration of these systems can lead to improved clinical outcomes across different healthcare settings, offering a holistic approach to patient monitoring. This process not only improves the accuracy of diagnostics but also supports better-informed treatment plans.